
Dagmara Sprudza, Zanna Martinsone, Anita Pike
Rigas Stradins university, Dzirciema Str.16, Riga, Latvia, LV1007+37167409187 / dagmara-IOEH@rsu.lv
ABSTRACT
ABSTRACT
Within the framework of the National Programme (ESF) a study “Work conditions and risks in Latvia” has been carried out. During the study, health and social care employees (n=967) were inquired by questionnaire, work environment and work ability index analyzed. The results of the survey show that work conditions are not sufficiently reliable and healthy - 32% of risk factors exceeded occupational exposure limits or recommended value. The respondents frequently mentioned thermal discomfort, draught, dry air, noise and insufficient lighting, shortage of time, overtime work, long working hours, handling of heavy patients, awkward posture and repetitive movements, psychological disagreement, menace. In recent years number of occupational diseases among medical and social care employees has rapidly grown. 29% of the respondents evaluated their working capacity as good.
Keywords
health and social care employees, risk factors, occupational diseases, work ability index.
INTRODUCTION
INTRODUCTION
Our rapidly changing living environment is closely related to changes in work environment – work becomes more intense and requires maximum attention and concentration, adaptation of work with mental and physical capacity of an individual, as well as dealing with different managerial issues. At the same time, traditional work environment risks still exist – noise, vibration, dust, chemical substances etc.[1,2,3] In Latvia no noteworthy and wholesome studies have been carried out, which could reveal occupational health and safety situation in Latvia and could help in decision making. It would be reasonable to consider existing situation, as well as historic, economic and social specifics, which differ a lot among countries, regardless the unified European Union requirements. It should also be noted that in Latvia no single national strategy in occupational health and safety has been approved, which would include priorities, objectives to be reached in future, as well as justified solutions to existing problems and necessary changes in the field of occupational health and safety. Thus, objective of the Study “Work conditions and risks in Latvia” was to create analytic base in the field of occupational health and safety, which would ease rational and effective decision- making for elaboration of employment and social policy programmes and for ensuring sustainable development [4].
MATERIALS AND METHODS
The Study “Work conditions and risks in Latvia” is comprised by several activities and various working methods. Combination of methods ensured obtaining of both objective information and subjective opinion of different interested parties regarding occupational health and safety situation and legal labour relations in Latvia. The obtained results give a more realistic view on situation in Latvia, as well as changes that have taken place during the last ten years.
During the study following groups of people were surveyed (n=967): from hospitals (79%), out patient clinic (4,5%), care centre (3,9%), Social health agency, emergency medicine centre, social service etc. (12,6%). Totally were inquired :
− 280 doctors− 529 paramedics;− 39 junior medical staff.
Acquired results were compared to the results of survey of 2002.
Activities of the study included analysis of available occupational health and safety data bases, analysis of existing studies, objective assessment of occupational health and safety situation, using a database of measurements carried out by Hygiene and Occupational Diseases Laboratory of the Institute of Occupational and Environmental Health of the Riga Stradins University – in the period of 10 years 924 measurements have been performed.
Health and social care workers (n=746) were selected for work ability index assessment due to several reasons: there is comparatively high number of occupational diseases and workplace accidents in this group, occupational health and safety problems within this group have been widely studied all around the world, including studies regarding work ability index. Assessment of work ability index was elaborated as a research method by a multi-disciplinary group of experts of the Finnish Institute of Occupational Health (5). Work ability index is an instrument used in occupational health monitoring to assess capacity of a worker to do the work. For assessment of work ability index an employee answers series of questions combined in a special questionnaire. Work ability index includes seven aspects:
➢ urrent work ability compared with the lifetime best,➢ ork ability in relation to the demands of the job,➢ umber of current diseases diagnosed by physician,➢ stimated work impairment due to diseases,➢ ick leave during the past year (12 months),➢ wn prognosis of work ability two years from now,➢ ental resources.
Considering these aspects and provided instructions, work ability index was calculated and work ability of an individual assessed.
RESULTS
The results of the survey show that work conditions of health care and social care workers are not sufficiently reliable and healthy and cannot be recognized as being good - shortage of time, overtime work, long working hours, handling of heavy patients, awkward posture, and repetitive movements. New and modern occupational risks have replaced the old and conventional ones, such as different psycho-emotional factors, new chemical substances.
On work conditions, awareness and risk factors of health and social care employees.
Risk factors of work environment, which affect or might affect healthcondition of health and social care employees, are the following:
- biological agents (B, C hepatitis, HIV/AIDS, causative agents of tuberculosis, German measles and other infectious diseases);
- chemical substances (medicines, anaesthetics ) etc.;
- ionizing radiation (rentgenologists, radiologists, X-ray laboratory assistants, dentists, etc.);
- physical exertion (e.g., moving of bedridden, old patients);
- mental overload (long working hours, shift work, night work, taking several work loads, etc.) [6,7,8].
Nearly 90% (n=883) of the respondents note that they are informed on the harmful risk factors at work, but they are less informed about their effect on health - 83% (n=802) (see Table Nr.1).
Table Nr.1. Division by professions of health and social care employees regarding their awareness of harmful risk factors in their work environment and their effect on health
|
Type of information |
Allrespon -dents% |
Profession |
|||||
|
Order- lies % |
Assist. nurse% |
Nurses% |
Para- medic s % |
Doctors% |
Other% |
||
|
Informed on existence of risk factors |
89,8 |
91,7 |
86,2 |
88,0 |
87,9 |
92,2 |
91,1 |
|
Informed on effect of risk factors on health |
83,2 |
77,1 |
72,3 |
78,4 |
82,8 |
88,6 |
84,4 |
The main reasons for satisfaction with work are: social guarantees (68,8%), good relationships with colleagues (47,5% ), stableness of work (46,7% ), but safety and arranged work environment is noted by only 15% of the respondents. Whereas reasons for dissatisfaction are low salaries (55%) and great work load (41%). A quarter of respondents do not know who detects occupational diseases in Latvia. Level of awareness and understanding is still rather low.
In comparison to 2002, in the survey of 2006 respondents, in the workenvironment, find more physical exertion, biological, chemical and physical risk factors. Physical exertion as a risk factor is mentioned 2-3 times more often than in 2002.
As the cause of physical exertion is mentioned work in standingposition (often and continuously - 38%), prolonged stress of vision (often 35%, continuously – 33% of respondents) as well as strain of arms (often 40%, continuously – 23% of respondents). Frequent strain of arms is most commonly mentioned by doctors (31%).
Nearly one third of the respondents (32%) often lift heavy thingsweighing up to 15 kg, up to 20 kg -23%, but 50 kg and more - 38%.
Nearly one third (29%) of the respondents (paramedics and assistant nurses) within the period of last three years has had a trauma, when moving patients and heavy subjects. In 54% of the cases the employer was not informed on it.
Over half of the respondents (51%) are continuously exposed tobiological risk factors – microorganisms and viruses, patients’ blood, potentially infected needles. Only 60% of health and social care employees are vaccinated against viral hepatitis.31% of the respondents at work are continuously exposed to chemical substances harmful to the skin and respiratory organs (most often nurses and assistant nurses).
As the most common physical risk factors are mentioned: draft (35%),thermal discomfort (30%), insufficient lighting (26%), too dry air (25%) and noise (25%) - both impulsive and continuous.
PPI equipment (glows) usage has grown up to 30 % which is the positivesign of further education and information.
On objective condition of work environment
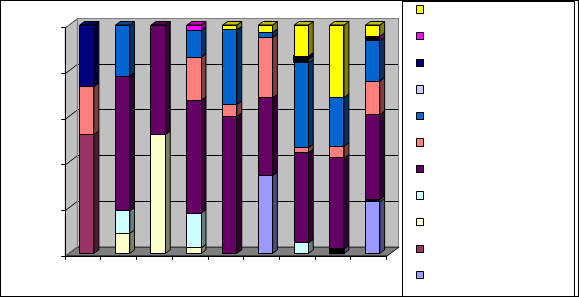
Number of objective measurements in the branch of health and social care has grown since 2002, which could be explained by adoption and implementation of state legislative documents (Fig. Nr.1). In 10-year period totally 924 measurements have been performed, most of all concentration of mercury vapours have been measured in stomatologists’ work environment, concentrations of lead and anaesthesia gases, measurements of microclimate and lighting performed.
In the measurements, 32 % (n=294) of evaluated risk factors do notcomply with occupational exposure limits (OEL) or recommended values.
Fig. Nr.1. Risk factors of work environment that exceed occupational exposure limits and recommended values (1998 – 2005)
 |
|
100%80%60% Lighting lx Cotton, wool, etc., dust mg/m3 Total microbiologicalpollution KVV/m3 Pollution with mould KVV/m3 Relative air humidity %40% Air temperature 0C Rate of air flow m/s |
20%
0%
1998 1999 2000 2001 2002 2003 2004 2005 2006
Lead mg/m3 Mercury mg/m3 Halotane mg/m3
Forane, izofluorotane mg/m3
The greatest deviation from the recommended values is observed in microclimate indices (29-55% (1999-2005)) and lighting (27%) (2005). Anaesthetic halotane exceeds OEL (1998) 22 times, but izofluorotane – 10 (2003) and 7 (2005) times. Concentration of lead and quicksilver in some years exceeds OEL. Comparatively small attention is devoted to evaluation of concentration of disinfectants in work environment.
The most common occupational diseases, incidence, accidents.
Occupational morbidity has been analyzed for doctors, paramedics and others. Occupational morbidity has soared in recent years, exceeding an average increase in other groups of employees (see Fig. Nr. 2).
Fig. Nr.2. The most common occupational diseases of all health and social care employees, divided by years per 100000 employees.
600
500
Infections and parasite diseases
400

300
Diseases of nervous system and sense organs
200
100
![]()
|
Respiratory diseases |
0
![]()
![]()
![]()
![]()
![]()
![]()
Years
Diseases of skin and subdermal tissue
![]()
The first place in the general structure of occupational diseases is taken by spinal spondylosis and radiculopathy, the second place – by syndrome of carpal tunnel and the third – by deforming osteoarthrosis in wrists. It should be noted that among paramedics the second place is taken by viral hepatitis C. Number of tuberculosis cases, related to work, has decreased during past three years.
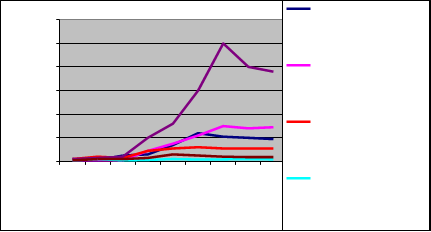
Population of health and social care employees is ageing (e.g., in 2000 number of working nurses at the age of more than 60 was 8% of the total number of nurses, but in 2005 it was already 12% of the total number of nurses).
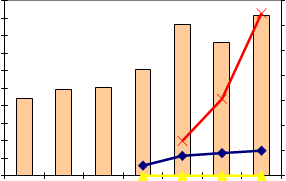
In the branch of health and social care, total number of accidents and numberof severe accidents per 100 000 employees tend to grow, lethal cases have not been reported (see Fig. nr.3).
Fig. Nr.3. Number of accidents per 100 000 employees in health and social care.
200,0
180,0
172,3183,4 70
160,0140,0120,0100,080,060,040,0
87,7
98,1 100,6
121,6
13,9152,1
30,8
9,165,0 60
50
40
30
2010,0
20,04,1 7,9 100,00,0 0,0 0,0 0,0 01999 2000 2001 2002 2003 2004 2005
Totally Severe Lethal Infection risk
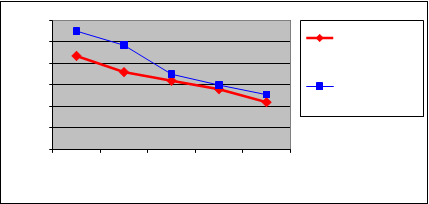
Majority of health and social care employees recognize their work capacity (work ability index-WAI) as good (7 and 8 points), and 29% of the employees consider their work capacity to be very good and evaluated with 9 and 10 points, however, at physical exertion working capacity is evaluated as very good or good by much less number of employees.
WAI at the age up to 40 among males was higher than among females, butafter the age of 40 it declines rapidly (see Fig. Nr.4).
Fig. Nr.4. Average WAI in relation to age and gender
424140
3838,7
|
36343239,737,237 |
36,4
36
35,6
35,1
34,4
Average WAI in females
Average WAI in males
3020-29 30-39 40-49 50-59 60 >
Age in years
Working capacity of health and social care employees in Latvia are significantly lower than in other European countries, particularly with regard to number of employees with excellent working capacity (WAI) [9,10 ].
CONCLUSION
Measurements of the work environment in health and social care area are not carried out frequently enough. The results of the Study indicate that there is a need to improve occupational health and safety legislation, as well as the system for interpretation of such legal requirements and building of public awareness. In spite of many informative – explanatory publications that have been issued in Latvia during the past 5-6 years, awareness of general public regarding provisions of the Labor Protection Law and regulations on occupational risk assessment, as well as other related issues, is dissatisfactory.
REFERENCES
- 1. M.Bake, D.Sprudza, I.Luse, N.Rusakova, I.Jekabsone (2003),.Risk assessment in medical institutions, Quo vadis Estonia 21Century?, Tartu, Estonia, 45.
- 2. M.Eglite, I.Vanadzins, R.Mangule (2003). Investigation of risk factors in the health care sector, Quo vadis Estonia 21Century?, Tartu, Estonia, 67.
- 3. M.A.Bake, D.Sprudza, I.Jekabsone, I.Vanadzins (1999). Health risk of medical personnel related to work environmental pollution. In: Proceedings of SECOTOX99 Fifth European Conference on Ecotoxicology and Environmental Safety. GSFBericht 02/99, ISSN 07211694, 402403.
- 4. EU Structural funds National programme “Labor market studies” project “Studies of the Ministry of Welfare” NoVPD1/ESF/NVA/04/NP/3.1.5.1./0003 “Work conditions and risks in Latvia”, (2007). Riga, ISBN 978998439233 2.
- 5. Tuomi K., Ilmarinen J., Jahkola A., Katajarinne L., Tulkki A. (1998), Work ability index, Finnish Institute of Occupational Health, Helsinki, ISBN 951 802202X, 34 p.
- 6. AhlbergHulten GK. Theorell T., Sigala F. (1995). Social support, job strain and muskuloskeletal pain among female care personnel. Skand. J of Working Environment and health, 21 (6), 435439.
- 7. Hignett S.(1996). Workrelated back pain in nurses. J of advancednursing. 23 (6), 123846.
- 8. Working Environment Survey (2000)
http://osh.sm.ee/research/emor_report.htm
- 9. HansMartin Hasselhorn, Peter Tackenberg, Bernd Hans Müller (2003). Work ability in the nursing profession // Working conditions and intent to leave the profession among nursing staff in Europe. Stockholm: Arbetslivsinstitutet, förlagstjänst, 8893.
- 10. H.M. Hasselhorn, P. Tackenberg, A. Buescher, M. Simon, A. Kuemmerling,
B.H. Mueller. Work and health of nurses in Europe - results from the NEXT- Study. // University of Wuppertal, University of Witten, 2005. www.next- study.net
Papers relacionados














