

Introduction
Conducting a Risk Assessment is a key to continuous improvement of quality and safety standards of any organization procedure. You must define the tasks, identify the hazards (facilities intrinsic characteristic, materials, procedures, situations, persons, which may cause damage) and assess risks (probability to occur a situation likely to cause damage and consequences) associated therewith and to which workers who are exposed. A risk assessment allows a diagnosis of work conditions, identification and/or quantification of risk and the determination of the corrections to be made, as well as preventive measures and more appropriate protection.
In a Nuclear Medicine department, despite the high degree of specificity, for being an area where ionizing radiation assume leadership as well as the Physicist role of responsibility in the department, is necessary and possible to conduct a Risk Assessment with the appropriate periodicity for a TSST or TST, so that security conditions could be verified on-site and the improvements that need to be made in order to not only minimize the harmful effects of radiation in the body, but also all other physical, chemical, biological and ergonomic risks in any healthcare department.
Nuclear Medicine is defined in a very simple and synthetically way, as a diagnostic and therapeutic technique that uses extremely advanced, safe and painless technology to produce images of body organs, allowing its visualization. Essentially allow us to obtaining scintigraphic images based on the ability to detect gamma radiation emitted by radioactive materials. This is a work area where ionizing radiations are constantly present, and is therefore essential to have a thorough knowledge not only of their consequences, as well as the preventive and protective measures to be taken. The existence of a Physicist is mandatory and crucial, not only to establish the criteria for the correct use of radioactive agents, as well as the patients and health professionals protection, regarding the application and use of ionizing radiation safely, among others.
Methodology
Specifications of a Nuclear Medicine Department
The main risks involved in a department of this nature are associated with the constant presence of ionizing radiation and consequent exposure. Ionizing radiation is characterized by having a higher frequency and a shorter wavelength as compared to non-ionizing radiation, but the main difference is that ionizing radiation has sufficient energy to transform atoms and molecules into charged particles, while non-ionizing radiation does not have enough energy to such a phenomenon. Examples of ionizing radiation are the x and gamma radiation, and non-ionizing radiation are infrared or visible light. Radiation exposure is associated with the act or condition of being subject to irradiation by radioactive sources or radiation emitting equipment, which can be external (irradiation by sources outside the body) or internal (irradiation by sources inside the body) [2].
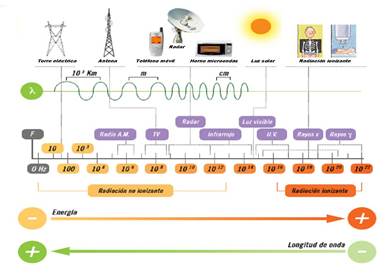
Figure 1. Electromagnetic Spectrum
According Avelar [1], Radiological Risk is a quantity measure that expresses the danger or the probability of adverse effects associated with a potential or actual exposure to radiation. Related quantities such as the probability of a particular harmfull effect, its intensity and its features. This risk may be due essentially to over- radioactive exposure, as well as the risk of contamination. Radioactive contamination is understood as the presence of radioactive substances in a medium or surface material. In case of contamination of the human body, this can be external when there is deposition of radionuclides on the outer body or internal, if the radionuclides penetrate the body through any via (inhalation, ingestion, wounds, etc.). [1].
The radiation can cause, directly or indirectly, excitation and ionization of atoms. Ions and free radicals are subsequently obtained and can initiate a sequence of chemical reactions which, in the case of living beings, have implications on the development, reproduction and cells viability. The biological effects depend on the nature and intensity of the radiation and the affected organ or tissue. It is important to highlight that natural radiation is the main source of radiation to which the population is subject and that it is not possible to distinguish the effects due to natural radiation from those originated by man [3].
The basic radiation protection standards are based on three general principles: Justification of exposure; Optimization and Individual Dose Limit:
1. Justification: No practice that leads to human exposure to radiation should be permitted, unless its introduction produces a beneficial effect.
2. Optimisation: All exposures shall be kept as low as reasonably achievable, taking into account economic and social factors.
3. Individual dose Limit: The effective dose should not exceed the recommended limits. The dose limits are based on the following assumptions:
- There is not a threshold below which there are no biological effects, ie any dose received involves a proportional hazard.
- Doses received on different occasions have cumulative effects. To determine the dose it shall take into account internal and external sources of radiation and should not, however, to this end, considerate the doses due to the natural radioactive background or appropriate medical examination or treatment (patients undergo medical examinations or radiation treatments with higher doses) [3].
The dose limits should not be considered as tolerance doses, because even the smallest dose has a certain risk.
Table1. Limits of effective dose or equivalent dose [3])
|
Directive 96/29/EURATOM |
Impl. Decr. 9/90 |
|
|
Exposed Workers (whole body) |
100 mSv for a period of 5 consecutive years, should not this value exceed 50 mSv in any single year |
50 mSv/year |
|
Crystalline |
150 mSv/year |
150 mSv/year |
|
Hands and feet or skin |
500 mSv/year |
500mSv/year |
|
Public (whole body) |
1 mSv/year (up to 5 mSv/year in a year provided that the average over 5 years does not exceed 1 mSv/year) |
5 mSv/year |
|
Crystalline |
15 mSv/year |
15 mSv/year |
|
Skin |
50 mSv/year |
50 mSv/year |
The Three Fundamental Principles of Radiological Protection and Safety, which should be permanently taken into account, are Time, Distance and Use of Barriers:
1.Time: the caused effects are directly proportional to the exposure time. A reduction of this time is an important factor to take into account in radiation protection. The exposure at a given point is directly proportional to the irradiation time:

The time factor is the primary method to limit the radiation dose.
2. Distance: The distance is another important factor in radiation protection, since the dose varies inversely as the square of the distance.
If kept constant all the emission characteristics of a radiation sources, time and all irradiation parameters, we will have the exposure at a given point varies inversely as the square of the distance between that point and the emitting source:

3. Barriers to use of suitable material: The choice of material depends on the nature of the isotope. For gamma radiation sources, the most widely used material is lead, although in the case of need for reduction of volume is replaced by a tungsten and copper alloy (17-18 g/cm3 density instead of 11.3 g/cm3) [3].

Figure 2. Lead Barrier
There are some general procedures that must be considered for the handling of radioactive sources, including manipulating the radiation so that the dose received by the handler is the lowest possible. For this it is important that all areas are limited to the dispersion of radioactive material; areas of handling radioactive material are marked; radioactive manipulations are carried out in areas covered by absorbent material and should be avoided unnecessary transport.
Individual protection measures for workers
The Personal Protective Equipments (PPE) are devices intended to be used to protect the user against risks which may pose a threat to health or safety. To effectively preserve the health and ensure the safety of persons and property, the personal protective equipment required to comply, in its design and manufacture, essential safety requirements and comply with the appropriate certification procedures and monitoring of its compliance with the essential requirements. These requirements and procedures set out in the Council Directive n° 89/686/EEC, of 21 December 1989, on the approximation of the laws of Member States relating to PPE.
Workers of a Nuclear Medicine Service shall comply with the following personal protection measures: use of proper clothing, do not use your mouth to pipette radioactive substances; avoid cuts or needle stick injuries, wear protection of syringes during preparation and administration of the radiopharmaceutical; label properly all radioactive material, to abandon the radioactive area, workers should carefully wash their hands, before leaving the workplace should be verified by the radiation detector, the clothing, hands or feet are contaminated.
To control the radiation dose to which he was exposed, he must always wear an individual dosimeter.

Figure3. Lead shields for syringes

Figure 4. Lead Needle Carrier

Figure 5. Personal dosimeter
The Basic Safety Standards for Protection against Ionizing Radiation and Security of Radioactive Sources were revised in 1994 and approved by the major international organizations (WHO, ILO, among others). Directive 96/29/EURATOM of the Council of Europe, of 13 May, determine the basic safety standards for the health protection of the population and workers against the dangers arising from ionizing radiation. One of the most relevant aspects of these standards and Directive is the emphasis on the recommendation of: “keep the exposure as low as reasonably achievable ionizing radiation, taking into account social and economic factors”.
As already mentioned, the presence of a Physicist in Nuclear Medicine Department is mandatory and essential, given the constant use of ionizing radiation. Their work contributes to the effectiveness of radiological imaging procedures, ensuring the safety of radiation and help in the implementation and development of optimized imaging techniques. It also establishes the criteria for the correct use of physical agents used in Nuclear Medicine, contributes to the development of therapeutic techniques and collaborates with oncologists for thec calculation of radiological treatment and monitoring plan and procedures on the equipment to ensure that patients receive a dose of prescribed radiation in the correct location.
The key responsibilities of the Physicist are to ensure and guarantee the safety and effective application of radiation to achieve a diagnostic or a therapeutic result prescribed for the patient, performing or supervising the procedures necessary to achieve these objectives. The Physicist responsibilities include the protection of the patient and other professionals in the application and use of radiation in a safety way; establishing adequate protocols to ensure patient dose and others; maintenance and characterization of radiation; determining effective dose; the development and implementation of the quality assurance program; advanced and necessary to ensure the image quality procedures; assist other health professionals in the application of radiation, weighing up their risk and their benefit.
The practice of Physicist translates into the use of physical principles and protocols to ensure the quality, quantity and application of radiation during radiological procedures. The term practice includes the calibration and characterization of radiation beams, quality assurance and management of equipments, the equipments specification, warranty and optimization of images and processing systems, the drawings of shields and analysis of radiation emission equipment and radiopharmaceuticals, the determination of absorbed dose to patients and those who are exposed to radiation, the radiation treatment plan, determining the dose to be administered in their respective fields, ensuring precise and specific radiation dose to each patient; help in drafting the requirements of imaging equipment (ie , gamma cameras) and additional equipment (cameras for safe and sterile handling of radiopharmaceuticals) and technical evaluation; acceptance tests of equipment sometimes in conjunction with the technical enterprises providers, development of the Licensing Process of installation refer to the General Directorate of Health, essential to be in operation.
The service in study is formed by a set of facilities properly prepared for this purpose. These facilities are located at ground level, complying with article 48 of DL 180/2002. Its location lies conditioned by risk type 2, according to Table VI of Article 83 of Annex VI to that DL. The facility has two distinct areas: active and non- active zone area. According to article 61 of DL 180/2002, the active area comprises the following areas: radiopharmacy, with its laminar flow camera, used for the preparation of all radiopharmaceuticals; transition area; administration of radiopharmaceuticals room; a waiting room for injected patients and their toilets; imaging area; reception, opening and storing radioactive products area; waste area; washing area. The department areas which are not considered as active zone are not active zone. The work team consists of two nuclear medicine technicians, two nurses, two physicians, a physical and two administrative techniques.

Figure 6. Gamma Camera

Figure 7. Laminar Flow Chamber
Data
“Risk assessment is the basis of the EU approach to prevent accidents and ill in health professionals. A proper risk assessment includes, among other things, ensuring that all relevant risks are taken into account (not just the obvious risks), verifying the effectiveness of the security measures, recording the results of the evaluation and review of assessment at regular time so that it remains up to date” (European Agency for Safety and Health at Work).
Among some steps considered by several authors, one of the possible sets of these same steps in the risk assessment process is the identification of hazards and those at risk; Assessing and prioritizing risks; Decision on preventive measures; the Adoption of measures; and, finally, the Monitoring and review.
This study was intended primarily to identify, estimate and assess the risk to the safety and health of persons in relation to its severity and probability, to obtain the necessary information for decision making on preventive actions that need to be taken. For this it was necessary to apply a method of evaluation for occupational hazards in order to design necessary preventive and protection measures. The intention was also to delimit the boundary actuation of Physicist and TSST or TST, whose functions are perfectly distinguishable and equally necessary.
The methodology and organization of work in the Nuclear Medicine department were observed during the study in order to be more perceptible the dynamics of it. Each element of the working group has its well-defined roles and responsibilities. The Nuclear Medicine technician prepares radiopharmaceuticals needed for scheduled exams. Thereafter, patients are greeted by Nuclear Medicine technician who performs a short survey before proceeding to the administration of the radiopharmaceutical, which is carried out by nurses. Images are acquired and also processed by Nuclear Medicine technician, and then be analyzed and reported by physicians, embodying the patient's diagnosis.
The Risk Assessment method chosen was MARAT (Method for Risk Assessment of Accidents), for being general, relatively complete, intuitive and easy to apply. In this method, it was determined the disability level, through checklists, which, together with the exposure level, allowed to determine the probability level, which, in turn, in conjunction with the Severity Level, enabled the determining the risk level and thus the control level.
A checklist, in which were registered the main activities and their associated tasks, was made.
 |
||||||||||||
 |
||||||||||||
 |
||||||||||||
|
||||||||||||
|
||||||||||||
 |
||||||||||||
 |
||||||||||||
|
||||||||||||
Figure 8. Risk Assessment Method – MARAT
Table 2 – Checklist example
|
Activity |
Task |
|
1. Radioactive materials handling (radiopharmaceuticals) |
1.1. Radioactive materials handling (radiopharmaceuticals) |
|
1.2. Storage of radioactive waste produced |
|
|
1.3. Procedures in the patients admission |
|
|
1.4. Organization of reports relating to the examinations |
|
|
2. Radiopharmaceuticals injection in patients |
2.1. Patients monitoring |
|
2.2. Injection of radiopharmaceuticals in patients |
|
|
3. Procedures in injected patients area |
3.1. Procedures in the area reserved for injected patients |
|
4. Image acquisition and processing procedures |
4.1. Image acquisition |
|
4.2. Image processing |
|
|
5. Cleaning |
5.1. Cleaning with use of chemical agents |
|
5.2. Working with cleaning machines |
Results and Discussion
After description, observation and daily monitoring of the work done in the Nuclear Medicine department, it was possible to complete the checklists prepared for this study.
In Activity 1, were detected to correct various situations, in particular task 1.1., due to the risk of radiation exposure, skin contact with chemicals agents or heavy objects fall (lead or tungsten), during handling. These risks can lead to carcinogenic effects, chemical burns or multiple injuries, respectively. A Control Plan was made, in which some constructive measures such as the presence of a sink in the transition area for Radiopharmacy, and organizational measures, such as implementation of a radiation protection plan and implementation of procedures for conducting tenders were prepared (specified in DL 180/2002). In task 1.3, tees hazards were identified: working with the monitor, stressful situations and work with the phone. The risks associated with these hazards are eyestrain or headache due to eye movements; headache or psychosomatic disorders due to mental fatigue; and musculoskeletal disorders due to shoulder elevation with cervical, respectively. In the Control Plan, organizational measures such as conducting increased health surveillance of all workers in the department and protection measures as the use of hands - free devices for phone, wherever possible, have been proposed for this task. For the task 1.4., were identified as hazards work with headset and the computer mouse/keyboard. The risks are, respectively, the auditory fatigue, which can cause disturbances of hearing, and flexion and extension of the wrist, which may lead to musculoskeletal disorders. In the control actions plan was proposed, as an organizational measure, conducting increased surveillance of the health for all workers in the department.
For Activity 2, several things could be improved, particularly as regards the monitoring of patients (task 2.1), due to the danger associated with physical exertion in case of need for transport of patients with mobility disability. The risks are excessive physical effort, which may lead to musculoskeletal disorders and stressful situations that can lead to mental fatigue or headache. The proposed organizational measures have been conducting increased surveillance of the health for all workers in the department and the implementation of written procedures for the organization and execution of the task. As for task 2.2, the dangers are ionizing radiation and biological agents. The risks associated with this are the ionizing radiation exposure, which can lead to cancer, skin diseases or headaches, and exposure to biological agents (such as viruses, bacteria, etc.), which can cause various types of infections. The organizational measures proposed were increased medical surveillance, implementation of written procedures for the organization and execution of the task and implementation of radiation protection plan. As a protective measure, was proposed acquisition and supply of PPE.
The dangers, risks, consequences and organizational measures proposed for Activity 3 are equivalent to the task 2.1, cited above.
For Activity 4, several operations were detected to correct for both tasks 4.1 and 4.2. The present dangers are ionizing radiation and monitor, mouse and keyboard work. The risks are exposure to radiation; flexion and extension of the wrist, whose injuries have been reported previously; and eye movements, which can lead to eyestrain and/or headaches. The proposed organizational measures are the implementation of radiation protection procedures and the organization and execution of a written task plan. As a protective measure, was proposed acquisition and supply of PPE.
For Activity 5, several operations were detected to correct for both tasks 5.1 and 5.2. The present dangers are related to chemical agents, when they come into contact with the skin can cause chemical burns and dermatitis, and the use of electrical equipment which, in case there is contact may cause an electric shock or burns or, in the case of an accident can lead to multiple injuries. The proposed organizational measures are training on manual handling and implementation of written procedures for the organization and execution of the task. As a protective measure, was proposed acquisition and supply of PPE.
Analyzing the obtained results, it is possible to determine some tasks that involve greater risk and some corrections to make. The risks associated with exposure to ionizing radiation must be corrected with measures such as the implementation of a radiation protection plan, written procedures for the organization and execution of tasks, enhanced medical surveillance, acquisition and provision of appropriate PPE. There are also ergonomic risks that can be improved /corrected with measures such as increased medical surveillance, use of hands free devices and implement written procedures for the organization and execution of tasks. Were also identified biological and chemical hazards that must be corrected with various measures, including the use of appropriate PPE, training or enhanced medical surveillance.
Conclusions
This study allowed the identification of risks associated with the hazards present in the Nuclear Medicine department, enabling appropriate prevention actions with implementation of MARAT method. It was important to know the rules on the health protection of the workers and the general public against the dangers arising from ionizing radiation contained in Directive N. 96/29/EURATOM.
The highest risk is posed by activities involving contact with ionizing radiation, such as the handling and storage of radioactive materials, radiopharmaceuticals injection or images acquisition in gama camera. The limited health surveillance and the absence of a written plan of radiation protection greatly increases the weighting of this type of risk. However, they also are present ergonomic, chemical and biological hazards, which cannot and should not be devalued. European data show that the percentage of workers in the health sector that believes that their health and safety are at risk due to the nature of their work is higher than the average of all sectors in the EU. Workers in the health care sector are, for example, the risk of injuries caused by needles or sharps that may lead to infection of blood borne pathogens (viruses, bacteria, fungi and other micro-organisms). The human immunodeficiency virus (HIV) and hepatitis B virus (HBV) or C virus (HCV) is the most common risk, but there are more than 20 diseases that can be transmitted through blood [2].
This work also enabled us to verify that the work of a TST or TSST in a department of this nature makes as much sense as any other. Admittedly, the Physicist is part of the working team of Nuclear Medicine, responsible for ensuring and guaranteeing the safety and effective application of radiation to obtain a diagnosis or prescribed therapeutic outcomes for the patient.
The Physicist responsibilities include the protection of patients and other professionals regarding the application and use of radiation safely; establishing adequate to ensure patient dose and other protocols; maintenance and characterization of radiation; determining effective dose; procedures to ensure the quality of the image; development and implementation of the quality assurance program; assistance to other health professionals in the application of radiation, weighing up their risk and their benefit.
However, as seen with this Risk Assessment, there is a whole range of risks that must be taken into consideration and that line is the scope of intervention of a TSST or TST.
Acknowledgments
A preliminary version of this paper has been presented at ORPconference 2014.
References
- 1. Avelar, R. (s /d). Course of Radiological Protection and Safety. Radiation Dosimetry. DPSR DGA. Lisbon.
- 2. Duarte, E. (2006). Report of the Working Group on Monitoring and Nuclear Safety. Brasilia.
- 3. Martinho, E., Salgado, J. (1996). Introduction to Radiation Physics. Ministry of Science and Culture. Lisbon.
- 4. Robin, M. J. Sousa, A. L. (1998). Fundamental concepts of imaging. Edt Lidel. Lisbon.
Papers relacionados














